The report of an independent inquiry into the United Kingdom’s contaminated blood scandal will be published, and Britain is expected to shell out more than 10 billion pounds ($12.70 billion) compensating thousands of people who were infected with HIV or hepatitis, British media reported.
UK’s Contaminated Blood Scandal
Why In News
- The report of an independent inquiry into the United Kingdom’s contaminated blood scandal will be published, and Britain is expected to shell out more than 10 billion pounds ($12.70 billion) compensating thousands of people who were infected with HIV or hepatitis, British media reported.
What It Is All About
- A shocking report released claims that a decades-long UK disaster, in which thousands of people died after receiving treatment with contaminated blood, was hushed up and mostly preventable.
- The inquiry was launched six years ago in 2017, when Theresa May was Prime Minister. The inquiry was expected to look into how tens of thousands contracted the deadly diseases from transfusions of infected blood products in the 1970s and 1980s.
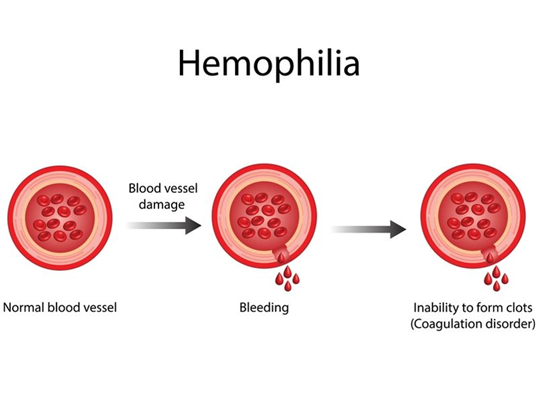
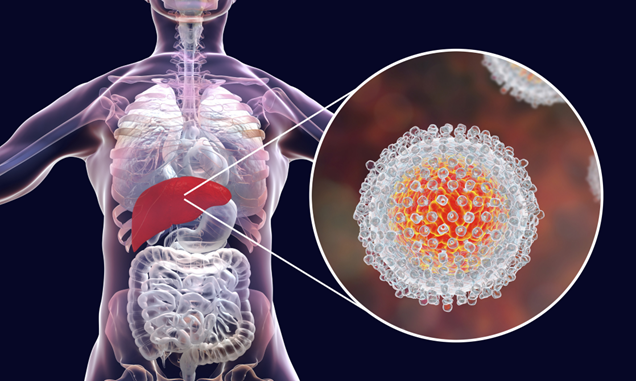
- The During the 1970s and 1980s, thousands of people who had the blood-clotting disorder haemophilia, were given blood donated or sold by people who were infected with the HIV virus and hepatitis. Tainted blood was also given to people who needed blood transfusions after childbirth or surgery.
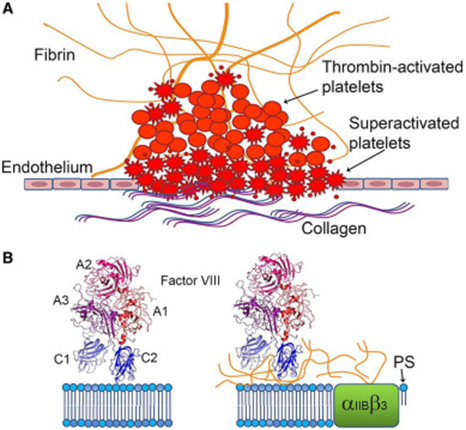
- In the early 1970s, the NHS started using a new treatment for haemophilia called Factor VIII. This was a processed pharmaceutical product that was created by pooling plasma from many donors. Factor VIII was considered to be a “wonder drug” for patients with classical haemophilia and Von Willebrand Syndrome (which is a bleeding disorder in which the patient’s blood cannot clot fully), more efficient and convenient than earlier treatments.
- The nature of Factor VIII was such that even one infected donor could compromise the entire batch of the protein. The product used by the NHS was imported from the United States, where a large volume of donated plasma at the time came from prisoners and users of intravenous drugs who were paid for their blood.
- The inquiry report has estimated that more than 30,000 people were infected with HIV, hepatitis C or, as in the case of 1,250 haemophiliacs, both. The Guardian has reported that most hep C infections were seen in transfusion recipients, and as many as 380 children were infected with HIV. Nearly two-thirds of those who were infected with HIV later died of AIDS-related illnesses, and an unknown number transferred HIV to their partners, a report by The Independent said.
- The report said that 2,400-5,000 recipients of blood developed hepatitis C, with the exact figure not known yet, as symptoms can show up years later.
- Several reports have stated that school children, some as young as 2 years old, were subjected to medical trials using infected blood products. The documents also showed that doctors in haemophilia centres used blood products, even though they were widely known as likely to be contaminated.
- As per the report, patients were “deliberately given Factor VIII, so they could be enrolled in clinical trials”. There is evidence that experts called on fellow doctors “to identify patients suitable for clinical trials” and more specifically, “previously untreated patients”.
- The 122 pupils who attended Treloar’s College between 1974 and 1987, 75 have so far died of HIV and hepatitis C infections.
- Another controversy of the time centred on medical trials that involved so-called “placebo” treatments — meaning that children who thought they had been given Factor VIII to prevent bleeds, had in fact been given a saline solution.
- With the belief that they could lead a near-normal life after the transfusion, these children engaged in rough outdoor games, only to risk their lives further.
- It was only after 1985 that all Factor VIII products were heat-treated to kill the HIV virus. However, UK blood donations were not routinely screened for hep C until 1991.
- Evidence provided to the inquiry suggests that the British government chose to turn a blind eye to the situation, mainly due to financial considerations. According to a BBC report, official documents from the 1990s showed that cost concerns prevented the NHS from pursuing adequate testing or campaigns to raise awareness, despite many warnings in the mid-1970s that blood donations from the US carried risk of viral infection.
- As early as 1953, the World Health Organisation (WHO), had warned of the hepatitis risks associated with the mass pooling of plasma products. It urged that dried plasma should be prepared from pools of between 10 to 20 donors to reduce the risk of contamination.
- In 1974, the UN agency warned Britain not to import blood from countries with a high prevalence of hepatitis, such as the US.
- Another warning of the risk of contracting HIV from blood products was issued in 1982. The following year, The Lancet and WHO said haemophiliacs should be told about the dangers of donated plasma.